I get asked all the time whether or not I recommend the shingles vaccine. Epidemiologists are saying that 1 in 4 people will get shingles in their lifetime. CDC (center for disease control) is recommending the vaccine for anyone over the age of 50 when it had previously been 60. I am not an anti-vaccine person but I am a know the facts before I get a vaccine type so I dove into this topic to learn more.
First, let’s look at what shingles is and why the vaccines were created to begin with.
Shingles, herpes zoster, originates from a prior chickenpox infection (varicella zoster) and belongs in the herpes family. This virus will be dormant in your body for many years and can emerge later in life as shingles. Shingles has a rather classic appearance of a line or cluster of small blisters that is on one side of the body only. Because herpes affects the nerve, they follow nerve patterns giving a distinctive appearance. Some people will have pain and itching at the site that later develops blisters while others just erupt with the blisters. Shingles can cause long lasting side effects particularly pain in the area of the breakouts called post-herpetic neuralgia (nerve pain). Post-herpetic neuralgia is the third most common cause of chronic neuropathic pain in the US. This pain can be very severe and debilitating lasting months to years. Shingles can also cause other side-effects (recall it is a herpes virus so many symptoms of the Epstein barr virus might be mimicked here). For example, it can cause a flu like syndrome, headaches, fever and malaise. About 1-4% of people who get shingles may end up hospitalized. A study estimated that there are an estimated 96 deaths per year with shingles as an actual underlying cause – these occur primarily in elderly people or those with significant impaired immune systems.
There are many theories of why people get shingles. When I was going thru medical school, if a young person (below the age of 60) got shingles we always had to work them up for AIDS because we only saw it in very immunocompromised people. This is not the case now. I am amazed at the number of young people who have had shingles. A decreased immune system certainly can contribute but it appears there is something else going on. The mandatory chickenpox vaccine has been blamed because with fewer cases of chickenpox, adults are not getting another exposure boosting their immune system. CDC disagrees with this theory and says the rise of shingles started before it was mandatory but epidemiologists think this is an important link and are concerned about the number of shingles cases in the generation receiving the chickenpox vaccine. (The chickenpox vaccine will have to be a completely different newsletter)
Two companies have created a shingles vaccine that are currently on the market. There are some important things to know and think about before you get this vaccine. READ ON to know what to ask and things to consider….
Zostavax by Merck & Co was the first vaccine on the market and was introduced in 2006. It is a live virus and this is very important to understand. A live virus vaccine has the potential of causing virus shedding, infection and transmission. In other words, it can actually cause shingles. Some side-effects might be categorized as minor including pain, swelling and redness at the injection site. But others may be more severe including fever, shock, joint and muscle pain, swollen glands, respiratory symptoms, severe eye infections that lead to blindness and even death.
The current recommendations for Zostavax is to give this vaccine to healthy individuals over the age of 60. The efficacy of the vaccine is approximately 51% for reducing the actual rash and a 67% for reducing the post-herpetic pain (neuralgia) associated with the shingles. Studies show a decline in efficacy of the vaccine preventing the post-herpetic pain during the first three years of vaccination from 67% to 31%. Zostavax was most effective in reducing shingles between the ages of 60-69 (64%) while only 41% for 70-79 and 18% for 80 and older. The CDC is no longer recommending this vaccine because of the declining efficacy but it is still available.
As of May 31, 2018 there have been 42,604 complaints of shingles reactions with 128 vaccine related deaths and 660 related disabilities. Merck has over 60 lawsuits pertaining to side-effects from this vaccine.
The new shingles vaccine, Shingrix, was released by GlaxoSmithKline in October 2017. Shingrix is a recombinant zoster vaccine (not live) and consists of TWO separate doses spaced out by 2-6 months. It is being recommended for individuals who are healthy over the age of 50. The efficacy for preventing a rash is close to 90% of all age ranges and between 80-90% for post-herpetic nerve pain. Shingrix studies show that protection stays 85% for at least the first four years after the vaccine (compared to 31% for the Zostavax). Efficacy has not been established for longer than four years.
A study comparing the two showed that Shingrix was 85% more effective in reducing cases of shingles than Zostavax but it carries a 30% increase in vaccine related side-effects. Shingrix side-effects can be severe and may be exacerbated if the vaccine is not given properly. If the injection is not in the muscle and ends up just under the skin significant local reaction can occur. In the original studies with Shingrix, 85% of the people receiving the vaccine reported local or systemic reactions such as pain, swelling & redness at site of injection, fatigue, headaches, etc and 17% reported more serious reactions preventing them from normal activities. Optic neuropathy and gout were also reported. When you dissect out the individual age groups, the age 50-59 group reported the following:
88% had pain at site of injection
57% had muscle aches & fatigue
51% had headaches
39% had redness
34% shivering
30% had swelling
In only 8 months of use, 3.2 million doses of Shingrix were distributed. As of june 30,2018 there were 4381 adverse events were reported to VAERS (vaccine adverse event reporting system). 3% were classified as serious.
Here are the important questions to ask your physician:
- What vaccine are they using? Zostavax or Shingrix? CDC is recommending the Shingrix vaccine over the Zostavax.
- What side-effects are they seeing? Shingrix causes pain and redness at the site of injection in most people and many people have muscle aches and fatigue for 2-3 days after the injection. They should disclose this.
- How do they administer the vaccine? It should be an intramuscular injection (not SubQ which is subcutaneous)
- What do you do if you have a reaction to the vaccine? Specifically, how to handle the swelling and redness if you get the Shingrix vaccine.
Who should NOT get a shingles vaccine?
- If you have ever had a severe allergic reaction to the vaccine
- If you currently have shingles. Once the shingles episode is over you can.
- If you are pregnant or breastfeeding
- Have a severe illness (especially at the time of injection)
- If you take antiviral drugs like acyclovir, famciclovir or valcyclovir then you must stop these drugs 24 hours prior to vaccination and not take them for 14 days after. Please do this under the supervision of your physician giving the vaccine.
Of note: If you have had the Zostavax vaccination before, CDC is recommending that you can have the Shingrix vaccine also.
Now, comes the tough question. Should you get the vaccine?
The only way I know how to dissect that out is to start with your risk of getting shingles and more importantly, what is your risk of the post-herpetic nerve pain because that is a significant cause of issues. There are several risk factors:
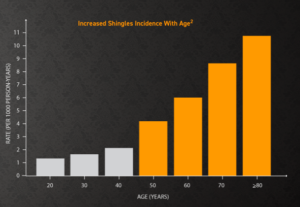
- I found a chart showing the incidence of shingles by age. This is from GlaskoSmithKline’s site but it appears to align with the data I found in other places. Of note, more than 50% of cases of shingles are in the 60 and older age group. There is a 1 out of 4 lifetime risk of getting shingles with the oldest age group of 80 and higher having a higher incidence of the post-herpetic neuralgia. See chart below..
- Presence of other medical issues: this increases your risk of the post-herpetic nerve pain from 5% upwards to 20%. Diseases like lupus, diabetes, recent trauma and low immune system (immunocompromised) all increase this risk.
Can shingles be treated if I don’t get the vaccine?
The current recommendations are to start antiviral therapy as soon as possible to try to prevent the post-herpetic pain. The medication may shorten the course of the shingles but doesn’t resolve it. If you have pain and abnormal sensations prior to onset of the rash, presence of >50 lesions and ophthalmic involvement your risk of developing the post-herpetic nerve pain is higher so be sure and take the medications. Once you get the pain, there are a variety of medications that are used with varied success.
My quick take home points on this vaccine that I deduced and would consider before getting the vaccine:
Be ready for side-effects so don’t get the vaccine before an important event.
The older you are the higher the risk of getting shingles.
Do you have any risk factors increasing your risk of getting shingles or the neuralgia?
My concern that I will actually voice out loud…. If the efficacy declines each year after you get the vaccine and the highest incidence of getting shingles doesn’t occur until after the age of 60…. What are we gaining by getting this vaccine in our 50’s if we don’t have any of the other risk factors? Hmmm. If you are in that 50 age group, it doesn’t mean you don’t get the vaccine it is just something to think about.
My other personal thoughts on “new” anything, is I like to see a track record before I jump in. Shingrix was released in October 2017 but it did have a median follow up of 4 years of data prior to that release in their studies. When you start doing things on a larger scale is when you really start to see how a product will perform. Again, I’m not saying don’t take the vaccine, I just want you to think about these things before you jump in to anything new.
Now that you know more about the vaccine, hopefully you can make an informed decision!
To your health,
Laura









